Emergency preparedness and environmental hazards
The PHA’s responsibility for the statutory health protection function includes emergency preparedness, the development of public health emergency plans for major incidents, and support for trusts and other Health and Social Care (HSC) and non-HSC organisations as required.
These roles also include giving public health advice to HSC organisations, multi-agency partners and to the public on more ‘slow burning’ chronic environmental hazards issues that could pose a threat to the health of the population.
Within the health protection service, this function is delivered by the emergency preparedness and environmental hazards team (EmpEnh). Although individual team members have specific topic and lead responsibilities, the team works on a regional basis and provides cross-cover for all issues and areas.
The responsibilities of the team include:
- responding to public health emergencies (including chemical and biological) through the provision of robust local arrangements 24/7;
- providing an early risk assessment of the actual or likely impact these incidents may have on public health or public safety;
- ensuring that an effective ongoing public health response/advice is provided for chemical contamination or other pollution that could have an adverse impact on the health of the population;
- ensuring that out-of-hours contact and ‘on-call’ arrangements are maintained and that the provision of 24/7 public health advice is sufficient during an emergency response;
- establishing, running and contributing to a scientific and technical advice cell (STAC) as and when required;
- participating in multi-agency emergency preparedness and response as set out within the civil contingencies framework;
- working with the resources available to provide HSC organisations with emergency preparedness guidance, advice and training as required.
Priority areas
Development of a joint response emergency plan
The PHA may be involved in responding to a range of incidents that have the potential to impact on the wider health and well being of the public of Northern Ireland.
Regardless of the cause of the emergency, the role of the agency is mainly two-fold:
- Health protection staff are available 24/7 to provide immediate and on-going public health advice into an incident.
- In an unfolding incident, PHA staff will work with colleagues from the Health and Social Care Board (HSCB) and the Business Services Organisation (BSO) to jointly lead the coordination of the HSC response when an incident or emergency involves more than one Trust, but does not require cross-department or cross-government coordination.
The PHA/HSCB/BSO joint response emergency plan sets out the main arrangements for this joint response, thereby ensuring that the response of the three regional HSC organisations is coordinated and effectively managed.
Incident and consultation response
Members of the EmpEnh team have responded to a number of incidents in the past 12 months. These have included carbon monoxide poisoning, an unused tyre fire with a toxic plume, a severe weather event with heavy snow, subzero temperatures and water supply shortages, and chlorine gas at a swimming pool.
Throughout each of these unfolding incidents, PHA staff worked with multi-agency partners to coordinate a community-wide response. Our partners included the Police Service of Northern Ireland (PSNI); Northern Ireland Fire and Rescue Service (NIFRS); Northern Ireland Ambulance Service (NIAS); local councils; Health and Safety Executive (HSE); Northern Ireland Environment Agency (NIEA); Northern Ireland Water (NIW); Northern Ireland Housing Executive (NIHE).
The team also leads the statutory response on behalf of the Integrated Pollution Prevention and Control (IPPC) applications in respect of new and existing facilities which could have an impact on the health of the community. It is also consulted in respect of planning applications which could have a potential adverse health impact.
Training
The PHA has responsibility (DHSSPS Policy Circular HSC (PHD) Communication 2/2010) to work within the resources available to facilitate training of, and emergency preparedness exercises for, relevant staff across the HSC system and the DHSSPS, including promotion of training initiatives.
As such, in 2011 the agency embarked on an initial training programme within the three regional organisations. Further joint training is planned with Trusts and DHSSPS in 2011-12.
Members of the EmpEnh team also contribute to the Health Protection module within the master’s degree in public health, run by Queen's University Belfast.
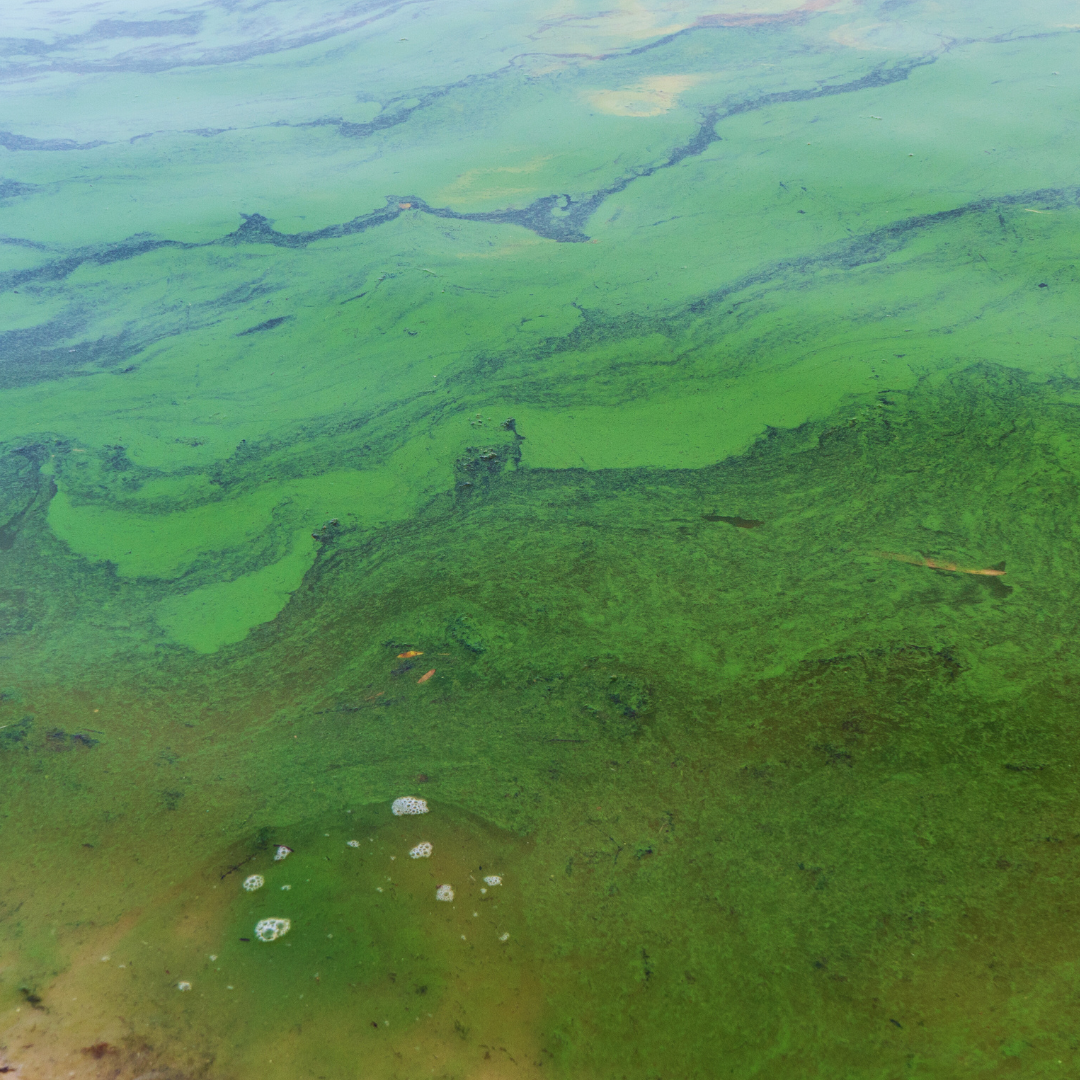
Blue-green algae - health risk to humans of blue green algae
Blue-green algae are not algae but a type of bacteria (called cyanobacteria) that are present in our lakes and rivers.
They are very small and can’t be seen with the naked eye. When environmental conditions are just right (they like warm still water with plenty of nutrients), they can multiply quickly forming a “bloom”
Blooms appear as a discolouration of the water (often a pea green colour) or as a visible scum layers or floating mats. Blooms usually occur in the summer and early autumn but can occur at other times of the year, if conditions are right.
There are no quick or easy remedies for the control of blooms once they appear in a lake or pond.
What are the health risks?
Blue-green algae may produce several different toxins which are harmful to human health. You may be at risk when you use a lake or other body of water which contains a bloom. You may be exposed during any activity where you may come into contact with the water, swallow water or breathe in water droplets for example swimming, sailing and boating, water skiing or even fishing.
These toxins can cause:
- Skin rashes,
- Nausea,
- Vomiting,
- Stomach pains,
- Fever,
- Headaches,
- Occasionally, more serious illness such as liver and brain damage.
How can the health risk be minimised?
Not all blue-green algae blooms are toxic but you cannot tell if a bloom is toxic by looking at it. If you see an algal bloom it is best to assume it is harmful and take the following precautions:
- Do not swim in the water
- Do not swallow the water
- Avoid contact with the algae
- Observe and abide by any warning notices positioned around the water
- For advice on eating fish caught recreationally from the water see the Food Standards Agency website Executive Summary - Microcystins in Fish | Food Standards Agency In respect of commercial fisheries, food safety advice should be sought from the district council responsible for the fishery. The district council may also liaise with the Food Standards Agency
Anyone who has come into contact with water containing blue-green algae should shower with fresh water immediately. If you have come into contact or drunk affected water and feel unwell you should obtain medical attention. Symptoms generally begin within hours after exposure.
Further Information
Blue Green Algae website - Northern Ireland has been experiencing an increase in blue-green algae blooms. To find out more about blue-green algae see www.daera-ni.gov.uk/blue-green-algae
NIEA are encouraging the public to get involved in citizen science and help monitor blooms of blue-green algae (cyanobacteria) to help protect public health and continue to enjoy our local water environment. Read more at www.daera-ni.gov.uk/news/help-protect-public-health-risks-harmful-blue-green-algal-blooms-bloomin-algae-app
Carbon monoxide poisoning
Carbon monoxide (CO) is a highly poisonous gas which is impossible to see, taste or smell. Anyone who uses an appliance that burns a fossil fuel including gas, oil and coal, as well as peat and wood, is potentially at risk from carbon monoxide poisoning.
Aside from deaths, many more people may suffer lasting damage to their health by lower level exposure to CO. This causes a series of flu-like symptoms, such as headaches, nausea, breathlessness, dizziness, collapse and loss of consciousness, to more serious conditions such as nerve damage, memory loss and personality change.
The PHA has responded to a number of incidents recently in relation to CO poisoning and issued several media statements. A letter was also sent to acute hospitals and primary care from the CMO (HSS MD 45/2010) in December 2010 urging HSC staff to remain vigilant to ensure recognition and prevention of further CO poisonings. The letter contains useful information about the risks of CO poisoning, how to avoid them, and how to recognise those affected.
The PHA in conjunction with the HPA in England also adapted a HPA algorithm for HSC professionals on how to diagnose and manage cases of CO poisoning. In November 2010, there was PHA input to the Health & Safety Executive’s advertising campaign, Watch Out: Carbon Monoxide Kills
The Public Health Agency is advising everyone to be aware of carbon monoxide poisoning. CO poisoning can be fatal and affect anyone. However, children, older people, pregnant women and people with heart or breathing problems are more vulnerable to its effects.
During the cold weather people across Northern Ireland will be turning up the heating and lighting fires, increasing their risk of CO poisoning. CO is produced when fossil fuels such as gas, coal, oil, wood, petrol and paraffin burn without enough oxygen. It is a colourless, tasteless, odourless gas that is non-irritating, and as a result can be very hard to detect, so people need to be particularly vigilant for the signs and symptoms of carbon monoxide poisoning.
Bad weather and snow can also mean gas flues get blocked by ice, causing an increased risk of carbon monoxide poisoning.
Symptoms include:
- headaches
- nausea and vomiting
- exhaustion
- drowsiness
- dizziness and light-headedness
- ‘flu like’ symptom
- palpitations
- chest pain
- losing consciousness
Carbon monoxide poisoning can be fatal and can also cause long-term health problems if victims are exposed to low doses over a long period of time. The signs and symptoms of carbon monoxide poisoning are often mistaken for other illnesses, such as food poisoning or flu – the symptoms can be similar to flu but without a raised temperature. Please look out for these signs and symptoms and consider if carbon monoxide poisoning could be the cause.
Anyone who suspects they may be suffering from carbon monoxide poisoning should immediately turn off all appliances, go outside and seek medical help from a qualified healthcare professional. Appliances should not be used again until they have been serviced by a registered engineer.
Carbon monoxide poisoning causes a number of deaths and hospital admissions each year. It is vital that we are all vigilant to ensure that we are protected from its dangers. Advice on the risks and measures that can be taken to prevent carbon monoxide poisoning is available online from nidirect. It is essential that people take care when using appliances and ensure that they are safe and used in properly ventilated spaces.
To minimise the risk of carbon monoxide poisoning the PHA recommends the following:
- install an audible Carbon Monoxide alarm that meets British or European standards (BS Kitemark or EN 50291). These cost as little as £20.00 and can be purchased from large DIY stores and food retail stores. Alarms, however, should not be used as a substitute for regular servicing of appliances;
- have their fossil fuel and wood burning appliances - such as boilers, heaters and cookers - checked by an appropriately registered engineer;
- sweep chimneys and flues every year if you use solid fuel;
- if you are in rented accommodation ask your landlord to provide you with an up-to-date gas safety record. This is a requirement by law and is particularly important for students renting houses and flats;
- keep flues, air vents and grilles clear and ensure rooms are well ventilated.
Further information from the Health and Safety Executive for Northern Ireland can be found at:
https://www.hseni.gov.uk/topic/carbon-monoxide
Flooding - advice if flooding occurs
During adverse weather some areas may experience flooding, the Public Health Agency (PHA) is reminding people of the potential public health risks associated with flooding.
In relation to flooding, the main risk relates to injuries caused by hidden dangers under the water such as missing manhole covers or people falling into fast flowing waters. The stress and strain of being flooded and cleaning up can have a notable impact on mental health and wellbeing.
The risk of contracting illness is generally low. However, as it is not always clear whether water is contaminated or not, the public are urged to exercise caution and assume that flood water is contaminated.
The PHA reminded residents there are a number of precautions to prevent health problems if there is a flood situation in the home. These include:
- wherever possible try to avoid coming into direct contact with floodwater;
- do not let children play in floodwater;
- When cleaning up after a flood, wear rubber gloves , boots and eye protection, and wash hands afterwards
- wash hands after being in contact with flood water, sewage or anything contaminated by these;
- wash children’s hands regularly;
- clean toys that have been in flood water with disinfectant;
- cover cuts or open sores;
- don’t eat any food that has been in contact with flood water;
- clean all surfaces with disinfectant before any food is placed on them;
- contact your GP if you or a relative develops a stomach upset following flooding.
Avoid unnecessary journeys.
Check in on elderly neighbours and remain mindful of current COVID-19 guidance which can be found here.
Care must be taken when clearing up after flooding as there is a serious danger posed by carbon monoxide fumes from the indoor use of generators to dry out buildings.
If flooding occurs in your local area contact the Flooding Incident Helpline on 0300 2000 100 immediately. This service is available 24 hours a day every day of the year.
The Regional Community Resilience Group (RCSG) helps local communities prepare for and respond to weather related emergencies;
Severe weather
During adverse weather many people can experience a range of situations associated with the extreme weather such as cold and freezing temperatures, no electricity or mains water and flooding. The Public Health Agency (PHA) has compiled public health information to assist the public in these situations.
- Support networks for those affected by the adverse weather
- Keeping warm during adverse weather
- Looking after vulnerable and elderly neighbours
- Carbon monoxide poisoning
- Advice if flooding occurs
- Using emergency water supplies
- Water advice following restoration
Severe weather warnings
The Met Office's severe weather warning page provides up-to-date information about weather that is likely to cause disruption.
The winter of 2010 saw the longest spell of snow and subzero temperatures in Northern Ireland for many years. Staff within the PHA responded to the unfolding ‘rising tide’ emergency with HSCB, Trust and DHSSPS colleagues to mitigate any risks to the health and wellbeing of the public.
Daily conference calls were held with the Trusts, primary care and multi-agency partners. Specialist health protection advice was issued to the public throughout the incident:
Reduce the risk of harm in the cold weather
Look after yourself this winter
Advice to the public during the current water shortage
If you are considering embarking on a journey during bad weather, you should consult the Met Office for travel conditions: www.metoffice.gov.uk.
If you must drive during severe weather, make sure you are prepared for bad weather conditions.
For further advice see: https://www.nidirect.gov.uk/campaigns/be-ready-for-emergencies
Severe weather - support networks and resources
Below are some of the support services that are in place for anyone who feels worried or stressed at this time.
It's important to stay protected against a drop in temperatures. By keeping warm, you can help yourself stay warm this winter. You can find out more here; Staying warm in winter | nidirect
Information from the NHS on how to stay well in winter can be found at How to stay well in winter - NHS (www.nhs.uk)
Rural Support
Bureaucracy, family circumstances, health and finances can cause stress and anxiety. We offer a listening and signposting service for farmers and rural families in Northern Ireland. All calls are confidential and the helpline operates from 8am to 11pm, seven days a week (voicemail and support options available at all other times), phone: 0800 138 16778. Rural Support website can be accessed at http://www.ruralsupport.org.uk/.
Information on the Rural Support Networks and the Warm, Well and Connect programme can be found here; Warm Well & Connected Programme (costaruralsupportnetwork.org)
These five directories list the names, numbers and web addresses (where applicable) of organisations that offer services to help improve mental health and emotional wellbeing within each Health and Social Care Trust area; Directory of services to help improve mental health and emotional wellbeing | HSC Public Health Agency (hscni.net)
Lifeline
If you, or someone you know, is in distress or despair, call Lifeline on 0808 808 8000. This is a free confidential service, where trained counsellors will listen and help immediately on the phone and follow up with other support if necessary. The helpline is available 24 hours a day, seven days a week. You can also access the Lifeline website at www.lifelinehelpline.info.
Samaritans
If something's troubling you, then get in touch. We're here 24 hours a day, 365 days a year. Contact us on 116 123 or visit our website at http://www.samaritans.org/.
For more information on looking after your mental health and the support available across Northern Ireland can be found at www.mindingyourhead.info. You can also visit your GP for advice.
Additional resources
HPA compendium of chemical hazards
HPA poisons information service
HPA extreme weather events and natural disasters
HPA CBRN incidents: a guide to clinical management and health protection
Cold weather - keeping warm during adverse weather
Cold weather can have a serious impact on health, particularly for older people and those with heart and lung problems, as it increases the risks of heart attacks, strokes and chest infections.
The following advice can help you keep warm at home:
- the best way to keep warm is by wearing multi-layers of clothing and to wear a hat and gloves, even indoors;
- if you can’t heat all the rooms you use, it is important to heat the main living room to at least 18ºC (64.4ºF) if you can and also before going to sleep, heat the bedroom to this too. If you can, heat the rest of the house to at least 16ºC (60.8ºF).
- It is important to make sure your heating is safe and that your house is properly ventilated, to reduce the risk of carbon monoxide poisoning. If you have not done so already, you should install a carbon monoxide alarm (further advice available at NIDirect)
If your electric is working:
- set the timer on your heating to come on before you get up and switch off when you go to bed;
- in very cold weather set the heating to come on earlier, rather than turn the thermostat up, so you won’t be cold while you wait for your home to heat up;
- never use an electric blanket and hot water bottle together as you could electrocute yourself;
- if you have an electric blanket, check what type it is – some are designed only to warm the bed before you get in and should not to be used throughout the night;
- make sure your electric blanket is safe to use by getting it tested every three years.
You can help keep warm by:
- wearing plenty of thin layers, rather than one thick one is better at trapping heat
- putting on a coat, hat, scarf, gloves and warm non slip shoes or boots when you go outside;
- wearing clothes made of wool, cotton, or fleecy synthetic fibers;
- wearing bed socks and thermal underwear at night.
- eat warm food and take warm drinks regularly. Food is a source of energy which helps to keep your body warm.
- keep active. When you’re indoors, try not to sit still for more than an hour or so. If you find it difficult to move about, stretching your arms and legs can also help keep you warm.
During very cold spells particularly where there is risk of snow and ice:
- Make regular contact with vulnerable people and neighbours you know to be at risk in cold weather – ensure they have access to warm food and drinks and are managing to heat their home adequately
- stay tuned into the weather forecast
- ensure you are stocked with food and medications in advance (have deliveries or ask a friend to help if needed)
- take the weather into account when planning your activity over the following days. Avoid exposing yourself to cold or icy outdoor conditions if you are at a higher risk of cold related illness or falls
- discuss with friends and neighbours about clearing snow and ice from in front of your house and public walkways nearby, if you are unable to do this yourself
- if you must go out, dress warmly and wear non-slip shoes. Tell someone where you are going and when you will get back. Keep your mobile phone (if you have one) on you and charged
- if you are concerned about your own health or that of others, alert emergency services
Information on energy efficiency and ways to save energy can be found here.
You can find information on keeping warm and well and on Cold Weather Payments at the links below;
Cold weather - looking after vulnerable and older neighbours
Vulnerable and older people can find it difficult to get out to the shops or to keep their house adequately heated during severe weather. The PHA is encouraging everyone to watch out for neighbours, friends and those who may be more vulnerable during severe weather and check that they are ok.
Who to contact if you need further help
If you are worried about a relative or an older neighbour, contact your local council. There is also help and support from the charity Age NI. Its website has information on how to stay warm in winter which contains useful contact numbers and advice: www.ageuk.org.uk/northern-ireland
You can find a guide to keeping warm and well in winter here.
Age NI teamed up with Lady Mary Peters to launch an exercise programme aimed specifically at keeping older people moving during the COVID-19 pandemic. Move with Mary is a series of five exercise videos. You can also learn more here.
Stay Well at Home's newsletter aims at providing hints and tips to help you develop your own 'Take 5' plan to stay well, active and connected during these challenging times. You can read it here.
Emergency water - using emergency water supplies
The Public Health Agency (PHA) advises the public to boil emergency water collected from standpipes and bowsers during water shortages. This is particularly important where water is used for direct consumption, for example drinking, brushing teeth, making up baby formula and ice cubes.
Although the quality of the water is wholesome, the cleanliness of containers used to collect the water cannot be guaranteed. As a precautionary measure, people should boil and cool the water if they are going to use it for drinking, brushing teeth, to make ice cubes and other similar uses.
It is important that bottles and containers used to collect water are clean and suitable for containing drinking water. Don't use anything that previously contained products that can't be consumed as washing may not remove all of the previous product.
It is also important to maintain good hand hygiene, particularly before cooking food and eating and after using the toilet and changing nappies. The very young and elderly are particularly vulnerable. The PHA recommends the following advice:
• use any water you have for hand washing first before you use if for showering or bathing;
• use antibacterial hand gels or wipes, if you have them, if you don't have water immediately available to wash hands;
• to conserve water you can use disinfectant wipes to clean kitchen and bathroom areas in particular;
• be extra vigilant in supervising small children to keep their hands clean too.
Water restoration - advice following restoration
Following a burst pipe or the restoration of water supply NI Water have the following advice for customers:
- Customers may experience some discoloration of the water following a repair / restoration of water supply but NI Water will flush the network as appropriate. Discolouration will be short-lived, and running the tap for a while should help clear the private service pipe to the property.
- Water quality is a priority for NI Water and strict disinfection procedures are adopted during any repair and water samples will be taken following a repair to our water network.
- The level of chlorine in the water supply may be boosted temporarily. The amount of chlorine is carefully controlled and monitored at our treatment works and strategic points in the distribution system. Water quality samples are taken following burst mains repairs to ensure that a satisfactory water supply is restored to customers.
Further information can be found on https://www.nidirect.gov.uk/articles/water-services